Introduction:
Immunotherapy for breast cancer is a complex and diverse disease that affects millions of women worldwide. Traditional treatment methods, such as surgery, chemotherapy, and radiation therapy, have been the mainstays in combating breast cancer. However, recent breakthroughs in cancer research have led to the emergence of a promising new approach: immunotherapy. This innovative treatment strategy harnesses the body's immune system to target and destroy cancer cells. In this article, we will delve into the concept of immunotherapy for breast cancer, its mechanisms, and the groundbreaking progress it has made in the fight against this formidable adversary.
Understanding Immunotherapy:
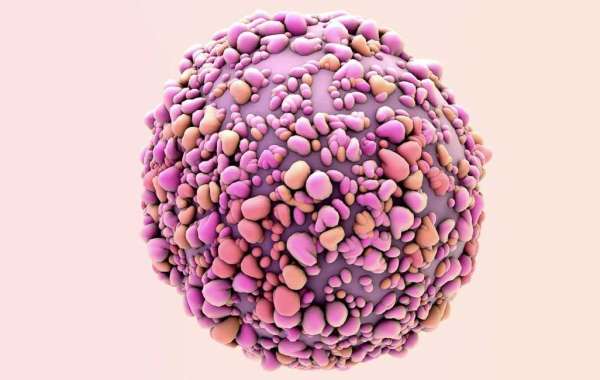
What is immunotherapy for cancer, also known as biologic therapy, is a revolutionary form of cancer treatment that mobilizes the patient's immune system to recognize and attack cancer cells. Unlike traditional treatments that directly target cancer cells, immunotherapy stimulates the body's natural defenses, enabling it to identify and eliminate cancerous cells more effectively. In the context of breast cancer, immunotherapy aims to boost the immune response against the specific characteristics of breast cancer cells, tailoring the treatment to the individual patient.
Key Components of Breast Cancer Immunotherapy:
Several types of immunotherapy are being explored for breast cancer treatment, with the most promising being immune checkpoint inhibitors, monoclonal antibodies, and cancer vaccines. Immune checkpoint inhibitors, such as pembrolizumab and atezolizumab, block the proteins that inhibit the immune system, unleashing its full potential to target cancer cells. Monoclonal antibodies, like trastuzumab, specifically target proteins on the surface of breast cancer cells, flagging them for destruction by the immune system. Cancer vaccines, on the other hand, stimulate the immune system to recognize and attack cancer cells bearing specific antigens.
Success Stories and Clinical Trials:
Immunotherapy has shown remarkable success in certain subtypes of breast cancer. For example, HER2-positive breast cancer, characterized by overexpression of the HER2 protein, has been effectively treated with targeted therapies like trastuzumab. Clinical trials are ongoing to explore the efficacy of immunotherapy in other subtypes, such as triple-negative breast cancer, where conventional treatments have limited effectiveness.
Combination Therapies and Personalized Medicine:
Researchers are increasingly focusing on combination therapies that integrate immunotherapy with other treatment modalities. Combining immunotherapy with chemotherapy or radiation therapy, for instance, may enhance the overall therapeutic effect. Additionally, the era of personalized medicine has allowed for tailoring immunotherapy based on the genetic makeup of the patient's cancer. This precision medicine approach ensures that treatment is optimized for each individual, maximizing effectiveness while minimizing side effects.
Challenges and Future Directions:
While immunotherapy has shown immense promise, challenges persist, including the identification of suitable biomarkers, managing immune-related adverse events, and extending the benefits to a broader spectrum of breast cancer patients. Ongoing research is focused on addressing these challenges and uncovering new avenues for enhancing the effectiveness of immunotherapy in breast cancer treatment.
Conclusion:
Immunotherapy represents a paradigm shift in the treatment of breast cancer, offering new hope and possibilities for patients. As research continues to unravel the complexities of the immune system and the intricacies of breast cancer subtypes, the potential for more targeted and effective immunotherapies becomes increasingly evident. The synergy between immunotherapy and other treatment modalities, coupled with personalized medicine approaches, holds the key to advancing the fight against breast cancer and improving outcomes for countless individuals around the world.